If the average person were asked to list the most common medical conditions plaguing Americans today, no one would be shocked to see heart disease, cancer or diabetes topping the list. However, most would be surprised to see hearing loss—affecting around 40 million Americans—take a top spot as one of the most prevalent chronic conditions in the nation.
Research shows that hearing loss negatively impacts almost every dimension of the human experience, including physical health, emotional and mental health, social and family relationships, as well as work or school performance. Even so, we tend to overlook the importance of treating hearing loss as a culture.3
The Physical & Socioeconomic Impacts of Hearing Loss
Hearing loss can have many causes, including genetics, exposure to excessive noise and aging.2 It can impact people of any age—from young children to senior adults and those in between. For example, almost 15% of kids ages six to 19 experience hearing loss from listening to loud music through earbuds.3 Those students with even mild hearing loss may miss as much as 50% of classroom discussion, significantly impacting their academic performance. Another 22 million working-age Americans are exposed to hazardous noise levels on the job, often resulting in long-term hearing damage.3
For the deaf and hard of hearing, the inability to communicate can dramatically impact everyday life, causing feelings of frustration, loneliness, and isolation, particularly among older people.2 Hearing impairment is also associated with comorbidities, including depression, anxiety, poorer cognition and physical health and increased falls.4
Hearing loss clearly results in big problems, but it’s treatable with the right intervention, most often through timely screening and the use of hearing aids. Meanwhile, data indicates people with hearing loss wait an average of seven years before seeking help.2,3 And while research suggests that almost 29 million U.S. adults could benefit from hearing aids, only 15% of older adults ultimately receive hearing screenings.1 Among those age 70 or older that could benefit from hearing aids, less than 30% have ever used them, and less than 20% of adults age 20 – 69 that need hearing assistance have ever tried a hearing aid.1 The average cost to a person with untreated disabling hearing loss is $9,100 per year.6
It’s not just about the medical issues hearing loss often causes for individuals. The consequences also ripple outward, resulting in a broader societal impact. People with unaddressed hearing loss experience higher rates of unemployment and are at greater risk for underemployment. Research shows that workers with hearing loss earn an average of $20,000 less than those who use hearing aids or cochlear implants to improve hearing.3 On top of potentially earning less and having less money to spend in the economy, the deaf and hard of hearing also see a 33% increase in medical expenses. If the individual doesn’t have health insurance, those costs are often passed on to the public.3
Common Obstacles to Obtaining Hearing Health Care: Cost, Health Care Disparity & Lack of Awareness
So, who is least likely to have health insurance or the income to address hearing care needs? While the gaps have narrowed in some areas over the years, large racial wage gaps remain across the U.S.
When looking at gender, race and ethnicity together, all groups’ average hourly earnings, except Asian men, lag behind that of White men. As of 2015, Black men were earning an average of $15 per hour and Hispanic men earned $14, compared to an hourly rate of $21 for their White counterparts.
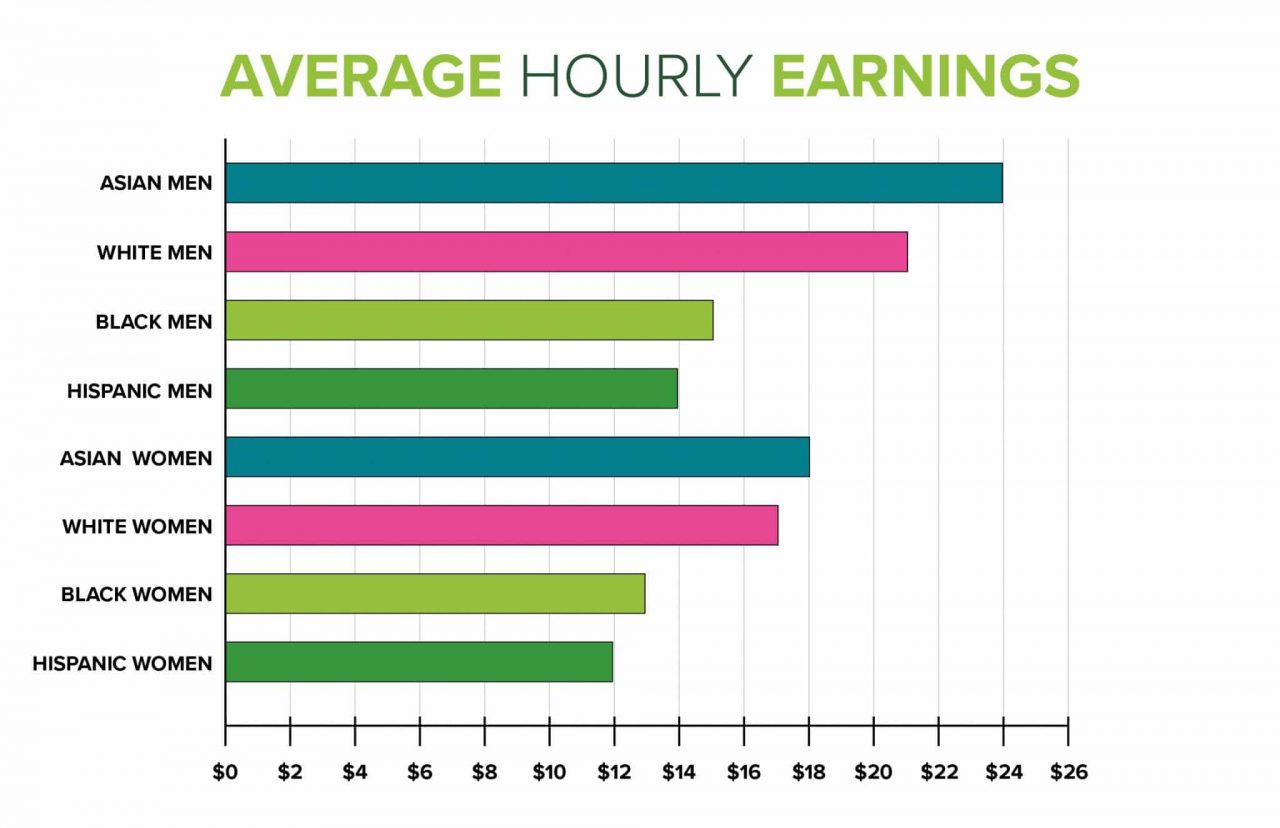
On the other hand, women’s earnings across all races and ethnicities lag behind both White men and the men of their own minority group. However, the average hourly earnings of Asian and White women ($18 and $17, respectively) are higher than those of Black women who earn an average of $13 per hour and Hispanic women making $12 an hour.10
Based on the wage information above, it should come as no surprise that many adults report cost as an obstacle to care. The affordability of health care is a significant issue in decisions about seeking care among those of lower socioeconomic status or those who live in rural areas. Research indicates homes with an annual family income of less than $35,000 are 10.6 times more likely to avoid needed medical care because of the cost than those with a yearly family income of $100,000 or more.9
With less economic flexibility, it can be challenging to afford the substantial financial investment required to buy hearing aids without the assistance of insurance (including Medicare).4 Generally, the cheapest hearing aids cost between $1,500 – $3,000, and the cost only goes up from there.7
Poverty, Unemployment, and Health Uninsured Rates by Race/Ethnicity
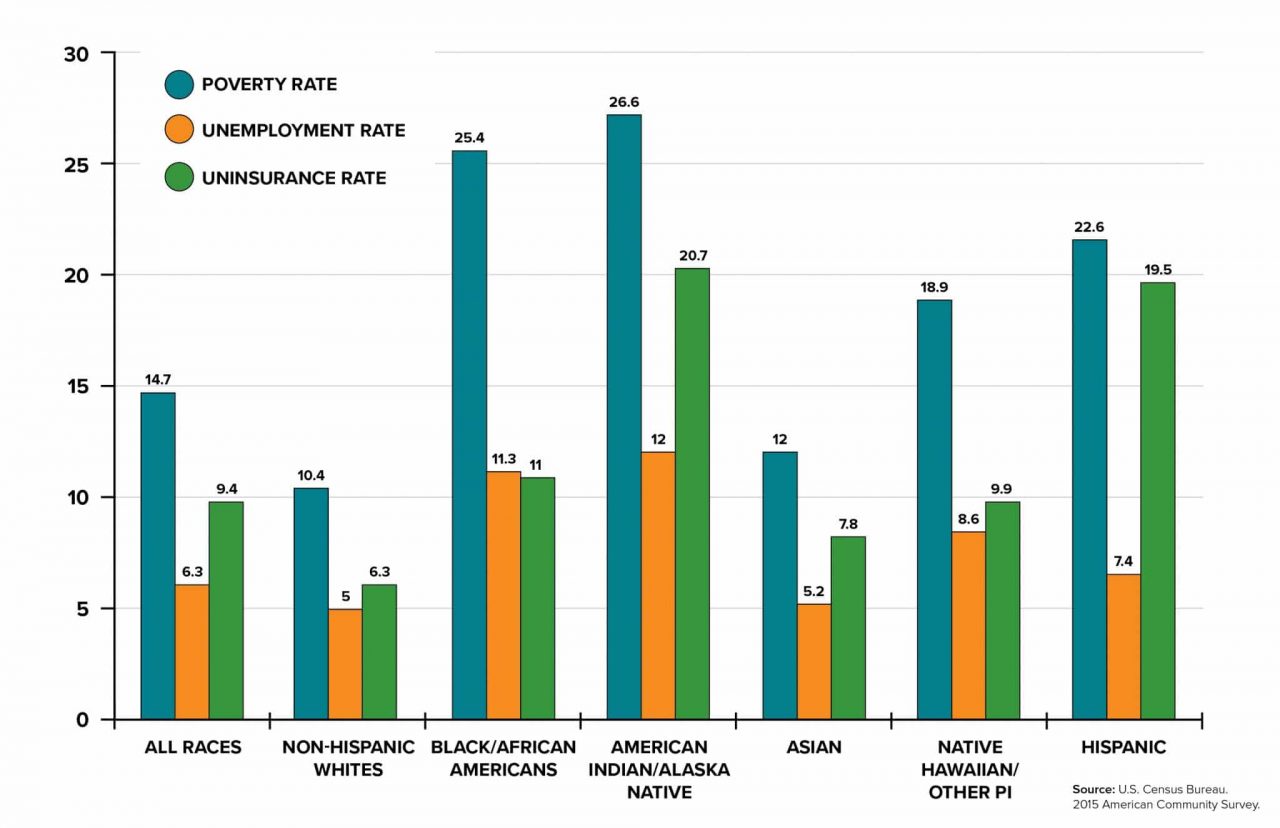
Many communities and minority groups also face significant disparity when it comes to accessing and using quality health care to address hearing loss. Compared with Whites, members of racial or ethnic minorities are less likely to obtain preventive health care and often receive lower-quality care.5 Individuals of lower socioeconomic status also experience more health care barriers and receive poorer quality care than higher-income individuals. Health care disparities also occur across other dimensions. For example, individuals living in rural areas face a range of access barriers from geographic location to lack of privacy and increased social stigma.8
However, treatment rates remain low even for those with hearing aid benefits. Even when a hearing impairment is identified, people still lack access to intervention services such as counseling, which results in an 83% gap in hearing aid need and use.2.4 A lack of public awareness and education around coping with the effects of hearing loss and inadequate management of hearing impairment as part of general health care is also a widespread issue.4 Treating hearing loss results in marked improvements in quality of life, job performance, relationship success and overall wellbeing.
Overcoming the Barriers to Healthy Hearing for All
Reducing health care disparities is essential from an equity perspective and improving population health and overall quality of care. In addition, health disparities are expensive. Estimates point to around $93 billion in extra health care costs and $42 billion in lost productivity annually across the country.8
Addressing the social factors and underlying policies or systemic issues that perpetuate inequality are crucial to ensuring hearing health and a better quality of life for all Americans.5 It’s estimated that around 50% of hearing loss cases could be prevented through improved public health measures that ensure early hearing assessment, prompt diagnosis and appropriate medical management. Policies are also needed to reduce noise exposure, raise awareness about hearing loss risks, and inform legislation designed to safeguard hearing.2
To date, many local and state governments, and the federal government, have not gathered, published or leveraged data on racial health disparities in ways that could drive productive action.5 Non-profits and public health agencies should prioritize partnering with health care organizations to measure health disparities among providers and within institutions to generate actionable insights into local care needs.
As health care providers, payers, lawmakers, and non-profits collaborate to increase health care access, it’s also important to question to what degree an approach addresses structural racism and equity issues. Failing to do so means that even the most creative solution may perpetuate inequity rather than prevent it.5
Finally, it’s also essential that decision-makers cultivate partnerships that empower patients to contribute to developing solutions. Non-profits and health care organizations would benefit from collaborating with community advisory boards or gathering patient-reported experiences and outcomes to identify potential care gaps and troubleshoot emerging problems. Successfully enabling patients to take ownership in the solution can lead to customized interventions rather than just amplifying mainstream methodologies and hoping for better results.
Today’s leaders must understand the differences in attitude, access to care, and culture of diverse groups and factoring those differences in developing significant health care initiatives.5
Bottom Line
With an estimated annual price tag in the billions, the consequences of untreated hearing loss can’t be overstated especially when considering that the most in need maybe already facing severe health care inequities. It takes a substantial social and economic toll on individuals and society when people are isolated from the surrounding world and access to their communities.
Treating hearing loss pays off in dividends—both for the individual and for society. Medicare and other health organizations have started to pay attention to the consequences of ignoring hearing problems or treating hearing care like an elective issue. As the population begins to live and work longer with an earlier onset of hearing loss due to increased noise exposure, untreated hearing loss impacts will only grow.
Increased outreach to educate politicians, leaders and the public on hearing loss—its causes, identification and prevention—is vital. Relieving the economic, social and physical impacts of hearing loss will also require collaborating across organizational, political and community lines to expand access to, and use of, quality hearing care for all.
Author
Brett Bachmann has been the CEO of Louisville’s Heuser Hearing Institute and Heuser Hearing & Language Academy since 2013. Under his leadership, HHI has significantly expanded its educational and clinical reach as the largest nonprofit speech and hearing center in the state of Kentucky to include five clinic locations in Louisville and Southern Indiana with nearly half of its thousands of patients being children.
End Notes
1 Quick Statistics About Hearing, National Institute on Deafness and Other Communication Disorders, December 15, 2016. https://www.nidcd.nih.gov/health/statistics/quick-statistics-hearing
2 Deafness and Hearing Loss, World Health Organization, March 1, 2020. https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss
3 Hearing Loss Facts and Statistics, Hearing Loss Association of America, May 2018. https://www.hearingloss.org/wp-content/uploads/HLAA_HearingLoss_Facts_Statistics.pdf?pdf=FactStats
4 Racial/Ethnic and Socioeconomic Disparities in Hearing Health Care Among Older Americans, U.S. National Library of Medicine, May 7, 2015. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4826391/
5 In Focus: Reducing Racial Disparities in Health Care by Confronting Racism, The Commonwealth Fund, September 27, 2018. https://www.commonwealthfund.org/publications/newsletter-article/2018/sep/focus-reducing-racial-disparities-health-care-confronting
6 Untreated Hearing Loss in the USA Costs $133 Billion Each Year, GlobeNewswire, February 25, 2019. https://www.globenewswire.com/news-release/2019/02/25/1741395/0/en/Untreated-hearing-loss-in-the-USA-costs-133-billion-each-year.html
7 How Much Do Hearing Aids Cost?, Consumer Affairs, September 28, 2020. https://www.consumeraffairs.com/health/hearing-aid-cost.html
8 Disparities in Health and Health Care: Five Key Questions and Answers, KFF, March 4, 2020. https://www.kff.org/racial-equity-and-health-policy/issue-brief/disparities-in-health-and-health-care-five-key-questions-and-answers/
9 Health Equity Report 2017, U.S. Dept. of Health and Human Services, 2017. https://www.hrsa.gov/sites/default/files/hrsa/health-equity/2017-HRSA-health-equity-report.pdf
10 Racial, Gender Wage Gaps Persist in U.S. Despite Some Progress, Pew Research Center, July 1, 2016. https://www.pewresearch.org/fact-tank/2016/07/01/racial-gender-wage-gaps-persist-in-u-s-despite-some-progress/